The dehumanisation of medicine
All HART articles also on Substack. Please consider a PAID SUBSCRIPTION so we can continue our work. Comments are open so you can join in the conversation.
Following the account from a frontline GP back in July outlining the woeful state of affairs within the NHS, we received a thoughtful response from another GP, confirming everything that was laid out, but also adding a few of their own thoughts.
We felt these further observations merited a separate piece:
Dear HART Group,
Thank you for the brilliant article by a frontline GP. I would echo and endorse every single word. I have been an NHS GP for over 30 years and am past NHS retirement age yet I can’t bear to abandon my patients to this inhuman system! I can help so few, but at least I can fight for them.
I have some further points to highlight that demonstrate how bureaucracy is obstructing proper patient care.
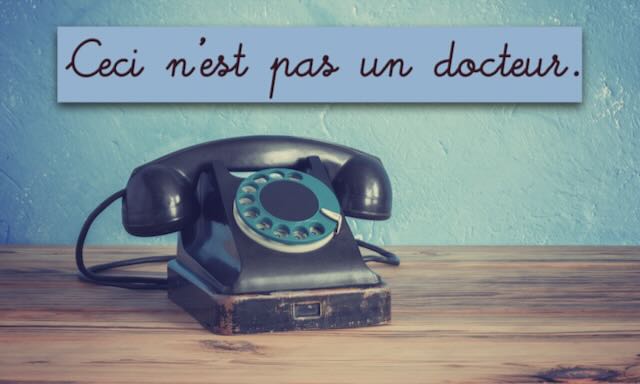
The inadequacy of telephone consultations
Far too many hospital appointments are still being conducted over the telephone. Recently, a cardiologist wrote to me to inform me that following a telephone appointment he had carried out with a patient, he wondered whether I would be able to see the patient in person to perform the examination that he couldn’t carry out over the phone! I was then to report my findings so he could adjust the patient’s medication accordingly. The obvious and less laborious answer would be for him to see the patient face-to-face in the first place, given the nature of the problem.
In other specialties, there is an initial phone appointment after which the specialist arranges the face-to-face that was needed in the first place. The outcome is two appointments instead of one, not to mention wasting valuable time which could have detrimental effects on patient outcomes. GPs have already effectively triaged these patients before referring and the need for a physical examination is inevitable.
Another frustrating loop of inefficiency is that elderly patients often don’t hear the phone, missing the call entirely. They are then marked as ‘did not attend’ (DNA) and have to be referred all over again. Equally often, they do pick up the phone but can’t hear or understand what the consultant is saying. A veritable merry-go-round of wasted resources and time.
The daily telegraph published an article on 29 November reporting on the worrying number of serious health issues being missed by telephone appointments. I personally went back to all face-to-face nearly two years ago and refuse to do telephone appointments except for repeat prescriptions and other purely admin matters. I think they are dangerous.
I can cite two examples immediately showing how incidental findings during a consultation can be more important than the problem the patient presents with. A few years ago I spotted a melanoma on the back of a patient’s arm when doing a routine blood pressure check. As a result, it was caught early and probably saved her life. Two weeks ago I saw a man with a minor knee problem. I took the opportunity to check his BP and pulse and found he was in atrial fibrillation. He had no symptoms. He needed anticoagulants to prevent stroke. These things would not have been picked up during a telephone appointment and both were life saving interventions.
Inability to make direct referrals
In our area, we cannot make direct referrals. Everything must first go through an ‘advice and guidance request’, even when it is obvious the patient needs to be seen. I’m happy for advice and guidance to be an option but this should not be a barrier to referring. This just wastes more time awaiting a response from the consultant. Once again, this is obviously not good for patient outcomes.
In our area, all physio, rheumatology and orthopaedics have to be referred to a Musculoskeletal Community Hub. The patient waits months to be seen by a physio then months again when the physio refers them on for the knee replacement, when they should have gone straight to the orthopaedic surgeon for a knee replacement in the first place.
Conclusion
When reading accounts such as these from frontline doctors, one is left with the most dystopian taste in one’s mouth. The whole setup seems to have been designed to waste time, resources, and maximise helplessness in sick people. These bureaucratic roadblocks certainly won’t help to reduce the week-on-week excess death toll that just rolls on, uncommented on by the previously doomsaying, podium-loving government of 2020 fame… or His Majesty’s Opposition, for that matter.
