
An assessment of the response to Covid-19
All HART articles also on Substack. Please consider a PAID SUBSCRIPTION so we can continue our work. Comments are open so you can join in the conversation.
HART has increasingly questioned the actual existence of any genuine pandemic in 2020. We have come to the conclusion that based on any sane definition of the word, there simply wasn’t one. However, we currently live in a world where this is a minority view. The eye-watering profitability of the ‘pandemic preparedness’ industry means we will likely remain in a minority for the foreseeable, due to the much discussed media-regulatory-institutional capture we now know to exist. With this caveat in mind, we can still discuss the UK public health response of 2020. Why did we throw out the entire rule book and implement the most disruptive and harmful replacement policies?
HART member Dr Alan Mordue, who spent most of his career working as a Consultant in Public Health Medicine, recently gave a talk to Common Knowledge Edinburgh on this topic. He directly compares what was in our pandemic plans before March 2020 and what we actually did in responding to Covid-19 in the context of some key principles of the specialty. His analysis makes it clear that these principles were abandoned during the pandemic, as were accepted codes on informed consent and even basic human rights. He ends with some high level lessons for the future and his talk is followed by a lively Q&A session (separate recording). Read his overview here.
Summary of CKE talk by Dr Alan Mordue
The Covid-19 pandemic was certainly a challenge for the Public Health system in the UK … so, how well did we meet it ? How could we improve our response, when inevitably, we face another pandemic in the future ? Before exploring these critical questions I want to first address the frequent and usually unequivocal assertion that we were not prepared for this pandemic.
Were we prepared for a ‘pandemic’?
As far back as 2009 the WHO produced guidance to encourage and support all countries to prepare for an influenza pandemic. The UK authorities also produced guidance in 2011 and 2013 and these documents were used by all local NHS organisations to produce pandemic plans, which were then reviewed and updated annually. The UK Influenza Pandemic Preparedness Strategy of 2011 explicitly said that these plans could be adapted and deployed for outbreaks of other infectious diseases, and gave as an example SARS. This key document also gave clear guidance about the general approach to handling a pandemic emphasising repeatedly that the response should be proportionate to the threat, and furthermore that:
“It will not be possible to halt the spread of a new pandemic influenza virus .. “, and
“During a pandemic, the government will encourage those who are well to carry on with their normal daily lives …”, and
“The response will continue to be evidence based …. based on ethical principles”.
After the last few years this approach seems revolutionary … even a little Swedish !?
Then in October 2019, just before the pandemic struck, the first Global Health Security Index reported on the adequacy of preparedness country by country and ranked the UK second in the world (USA first). Whatever problems there were in responding to the Covid-19 pandemic it would appear that they were not caused by a simple lack of preparation.
So … how did we do ?
Turning to the central question of how well we responded to the pandemic, I’ll consider this in relation to four key principles of Public Health:
| How did we do in relation to: 1 Ensuring accurate data on health & disease 2 Assessing evidence on the effectiveness of all interventions & their benefits and costs 3 Maintaining a broad focus on the whole population and all health problems 4 Providing accurate information to the public and avoiding unnecessary alarm |
1 Ensuring accurate data on health & disease
For the first two principles I have directly compared what was in our pandemic plans before 2020 and what we actually did in responding to Covid-19 (attached slides 7 & 8). At the outset the standard definition of a confirmed case was abandoned; until 2020 it was someone with symptoms of the disease in question plus a positive test identifying the likely causative organism … after March 2020 it became a positive test only. Not only that but the sensitivity of the PCR test was set too high (up to 40 cycles) and widespread community testing was undertaken, generating tens of thousands of false positives each week. Other changes to the usual way of defining hospitalisations and deaths were also introduced and all these changes exaggerated the scale of the problem, made it impossible to accurately monitor the developing pandemic, and helped to drive fear and an over-reaction.
2 Assessing evidence on the effectiveness of all interventions & their benefits and costs
Firstly I have compared the pandemic plans to the actual response for measures that aim to reduce transmission (see slides 9 and 10). These measures mainly comprise the much discussed non-pharmaceutical interventions (NPIs) and the plans recommended the following: isolating only those with active symptoms, minimal contact tracing, mask use only for healthcare staff, school closures only early in a pandemic if at all, and lastly “focused protection” of the vulnerable. The actual pandemic response tried to suppress viral transmission and could hardly have been more different, as we all know to our cost!
But what was the evidence for or against these two approaches ? Well … helpfully the UKHSA published a report in September 2023 entitled “Effectiveness of non-pharmaceutical interventions to reduce transmission of COVID-19 in the UK”. They reviewed 151 studies and concluded that “the body of evidence available … provides weak evidence in terms of study design …”, with only two randomised controlled trials, more observational studies, while the majority were modelling studies. It was a shame we didn’t have this report in March 2020 ! However, we did have a 2011 Cochrane systematic review and a WHO systematic review published in September 2019, just a few months before the pandemic started… and they reached similar conclusions. The latter said “The evidence base on the effectiveness of NPIs in community settings is limited, and the overall quality of evidence was very low for most interventions ….”. This review was also very clear that it did not recommend “in any circumstances” some all too familiar measures – contact tracing, isolation/quarantine of contacts, entry & exit screening at borders, border closures, and it did not even contemplate the lockdown of citizens in their own homes.
Moving on to measures to protect and treat individuals, let’s start by looking at vaccination, which for influenza was limited to health and social care staff and vulnerable groups, but for Covid-19 was eventually extended to most of the population despite limited evidence on effectiveness and safety. I address the effectiveness of vaccination in slides 15 and 16, and emphasise: firstly that data on major outcomes such as death or severe disease is more important than cases (the main outcome in the Covid vaccine trials); secondly, the importance of considering absolute risk reduction not only relative risk reduction (in slide 15 I’ve used the Oxford/AZ trial data to explain both and demonstrate the dramatic difference – 1.2% ARR vs 70% RRR); and thirdly, the importance of careful consideration of potential benefits for different sections of the population using ARR and the number needed to vaccinate (NNV) to prevent one death (note the optimistic assumption in slide 16 that the 70% RRR of cases will also apply to deaths !). Finally, these estimated benefits must be weighed against the incidence of known side effects such as VITT and myocarditis, the uncertainty on long-term side effects, and lastly the opportunity costs … and once again for each section of the population. It’s worth emphasising here that the data I’ve used in slide 16 to estimate ARR and NNV by age group were all available at the beginning of the vaccine rollout, and because of it I felt, and still do, that it was unethical to vaccinate healthy people below 60 years of age.
However, whatever decisions were taken by the JCVI and our governments on which sections of the population to offer Covid vaccines to, fully informed consent without any coercion should have been ensured. I show, in slide 17, the type of data that I believe patients need to be fully informed about a medical intervention, using as an example statins (to reduce risks from cardio-vascular disease). Chart 2 on the left shows benefits by age group (ARR) and is compared directly with the incidence of side effects on the right.
Last but not least slide 18 raises the vexed question of why early community treatment of high risk groups using re-purposed drugs was not supported, as well as the use of anti-virals and symptomatic clinical support for hospitalised patients.
3 Maintaining a broad focus on the whole population and all health problems
The transformation of the NHS into a Covid-19 service during the pandemic has been much commented upon with routine healthcare largely stopped, including cancer screening and even cancer treatment. However, not only did we almost exclusively focus on one condition but also on one section of the population to the detriment of others, particularly children. The response has also increased inequalities across the generations, across the working population, the public/private sector and across the world (slide 19).
4 Providing accurate information to the public and avoiding unnecessary alarm
We’ve already covered much of this but to summarise our pandemic response involved:
- inaccurate data on Covid-19 (by inflating cases, hospitalisations and deaths),
- mis-representing the effectiveness and harms from NPIs,
- mis-representing the safety and effectiveness of Covid vaccines, and finally,
- a deliberate heightening of fear and alarm to aid compliance.
This is quite a list and a serious indictment of the authorities, particularly our governments’ medical and scientific advisors !
So … what are my conclusions on how we did ? I’ve considered them in terms of “Process” and “Outcome” as shown below:
| So .. how did we do ? Process: * Abandoned fundamental principles of PH * Adandoned accepted codes on informed consent, introducing coercive measures to take vaccines * Adandoned fundamental human rights Outcome * Far higher excess mortality than Sweden * Excess mortality 2022/23 in post-pandemic period |
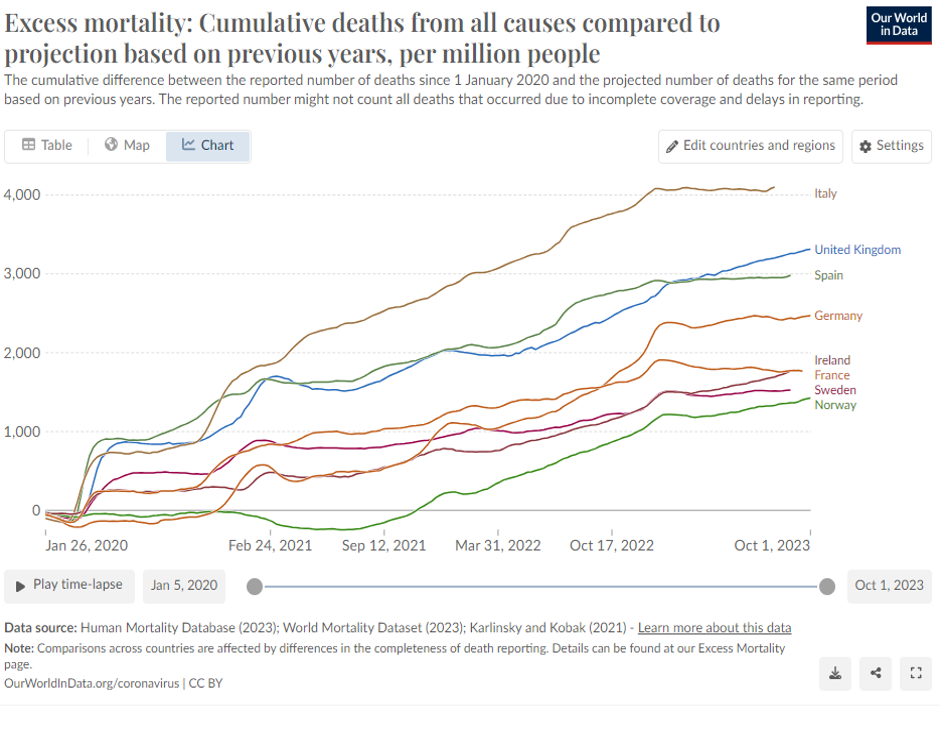
The evidence presented on the four PH principles seems clear, as is the mis-representation inherent in the vaccine mantra “safe and effective” and the coercive measures introduced to take the vaccine. Fundamental human rights were abandoned in terms of freedom of expression with widespread censorship and vilification of alternative views, freedom of movement and association with the NPI measures, and even the removal of the ability to visit dying relatives. Finally, turning to the outcomes, the chart below presents data from “Our World in Data” showing all cause excess mortality that is twice as high for the UK as Sweden and continues increasing up to October 2023, when in the 2022/23 post-pandemic period we should be seeing a fall or at least a flat line:
So what are the lessons for the future ? Well, I could go on at some length … but have confined myself to three high-level suggestions:
- Freedom of speech – the importance of an open and free debate within the medical and scientific community cannot be overstated, and is quite separate to the need for clear and unambiguous messages to the public at large during infectious disease outbreaks or pandemics. I believe the lack of such openness was the most fundamental mistake made during the pandemic response and underpins the abandonment of key principles and rights. If challenge and debate had been allowed the worst excesses of the Covid-19 pandemic response may have been avoided. In future pandemics and emergencies we must avoid all types of censorship.
- Fully informed consent – we must also re-commit to ethical codes on informed consent, including never using coercive measures whatsoever, and improving how we assemble and present information to patients to help them reach a decision.
- Maintain sovereignty and democratic accountability – this relates on the one hand to a more careful and limited use of emergency powers so that parliamentary challenge is not bypassed; and on the other to not handing over sovereignty and democratic accountability to an unelected international body that hardly covered itself in glory during this pandemic, namely the WHO (relates to the WHO Treaty and amendments to the International Health Regulations now being negotiated).
Web-links
- CKE
- WHO 2009 pandemic guidance
- UK Pandemic Strategy 2011
- GHSI 2019
- UKHSA review
- Cochrane 2011 review
- WHO 2019 review
