
Was it really eradicated, or just rebranded?
All HART articles also on Substack. Please consider a PAID SUBSCRIPTION so we can continue our work. Comments are open so you can join in the conversation.
The primary beliefs of vaccinology are that it is possible to educate the immune system to protect against disease, that vaccines are safe and that Smallpox was eradicated. It is quite possible to be very confident about the first points and still be able to question the evidence for the last one.
The Smallpox vaccine story is very well known. A modern medical miracle. The story we are told of Edward Jenner inoculating a child with matter from lesions on a dairymaid suffering from cowpox in 1796 in order to provide immunity to catching the more serious Smallpox is one which is taught to every child. Smallpox vaccination was given to every child in the western world in a WHO-led programme commencing in the middle of the 20th century, and after a few decades Smallpox was declared to have been eradicated from the face of the earth. Hurrah for modern science.
However, there are a number of questions that are worth asking about that story. A key question is whether the WHO were completely honest about their diagnoses. Curiously, just as Smallpox disappeared Monkeypox arrived. According to this WHO article, “The monkeypox virus was discovered in Denmark (1958) in monkeys kept for research and the first reported human case of mpox was a nine-month-old boy in the Democratic Republic of the Congo (DRC, 1970). Mpox can spread from person to person or occasionally from animals to people.”
Smallpox and Mpox are clinically indistinguishable from each other and the WHO’s claims of diagnosing a new pox were based purely on highly subjective laboratory testing (see below).
Even if we put all our faith in the WHO these “new viruses” are just filling an old ecological niche. In the same way as covid filled the influenza niche for a time such that covid replaced deaths that would have otherwise occurred from influenza.
What was Smallpox?
Smallpox was an infectious disease which produced a fever and, within a couple of days, a characteristic pustular rash, notably on the palms and soles of the feet. It was categorised into multiple subtypes even though the same virus was the cause, whereas in fact it is likely that different host responses were actually responsible for the differences. Accordingly, the case fatality rate could be anywhere from 1% to 90% depending on the “subtype”. However, looking at whole population data the rate was much lower than often quoted. For example in the 1700s the case fatality rate for the whole of Boston (around 10,000 people at the time) during each epidemic was reportedly around 10%.
Furthermore, the case fatality rate is highly dependent on the propensity to diagnose cases. Where mild cases were included, the case fatality rate plummeted; this propensity to hugely overestimate severity by only considering the cases which are brought to the authorities’ attention is a feature we still see with all infectious diseases.

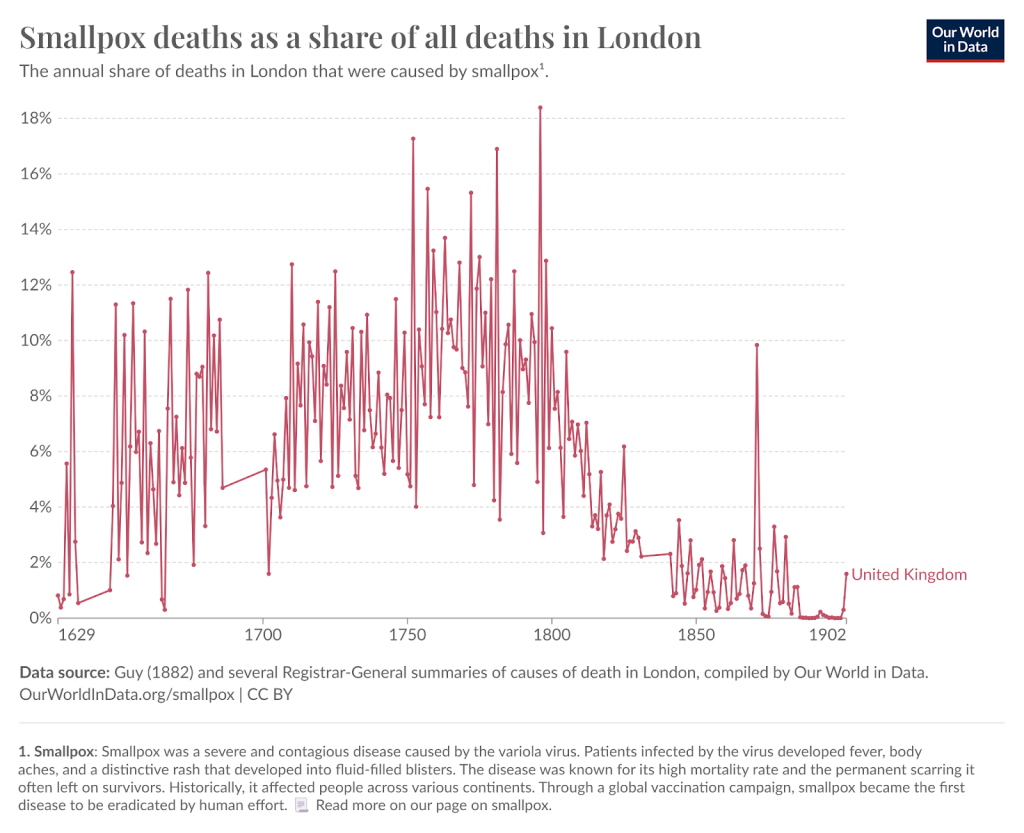
Smallpox was recorded as a cause of death in between 5-20% of ALL deaths in the 1700s in London (see figure 2). However, it has been present and killing people since the 6th century, albeit implicated in a much smaller fraction of deaths. That people were more at risk in urban areas raises the question of the role of sanitation, nutrition and other background health factors in keeping Smallpox at bay.
The claims that vaccination caused the massive fall through the 1800s demand a certain amount of scepticism. Variolation was practised widely in the 1700s, a practice where pus from Smallpox sores were inserted into an incision in the skin of healthy people. Vaccination was first introduced in the late 1700s when it was transferred arm to arm as fresh pus. Victorians admitted this was spreading syphilis and the technique was switched to using serum collected from infected calves in liquid form at a time before refrigeration was available, meaning that (even if there was any active ingredient) it was unlikely to have remained fully effective or sterile. Notably, the WHO was insistent in 1968 that “liquid vaccine undergoes rapid deterioration at ordinary air temperatures.” Importantly this brought an end to variolation, but the methods used were highly questionable.
How did Smallpox disappear so suddenly?
In 1959 the WHO announced an intention to rid the world entirely of Smallpox, the incidence of which had already declined very substantially. The last cases of Smallpox to be found at that time were in pockets of rural Africa including in Nigeria, Ethiopia and Somalia. The WHO eradication programme involved a campaign of “ring vaccination.” Someone with pox was infectious for a week after the pox appeared and it was believed that gave plenty of time to successfully vaccinate their contacts. The campaign was declared a success with the last case reported in Somalia in 1977.
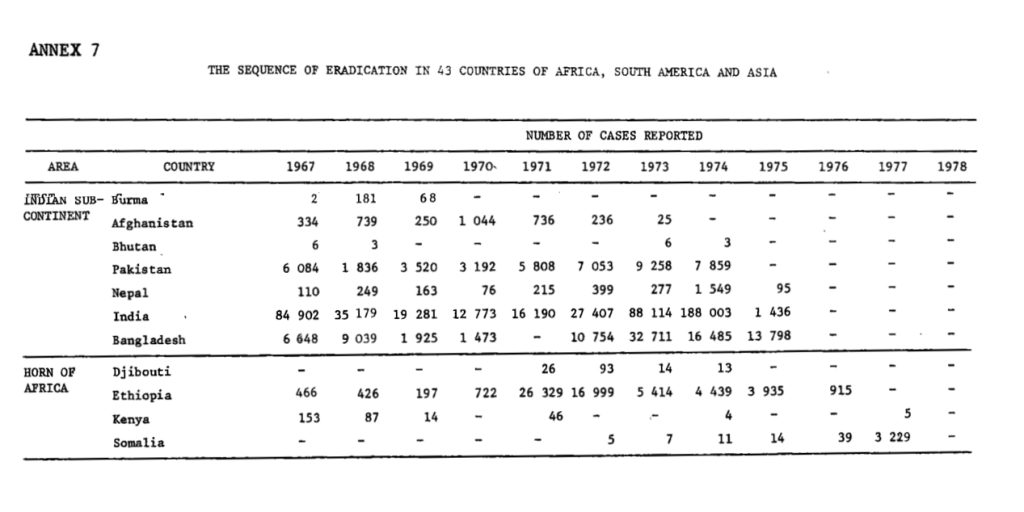
The number of reported cases reduced to a third of previous levels in the 1960s and 1970s before the abrupt announcement of total eradication of the disease. There were 3,234 cases reported by WHO in 1977, the last official year of Smallpox spread.
A WHO report from 1968 claimed there were around 60,000-120,000 cases reported each year from 1959 to 1967.
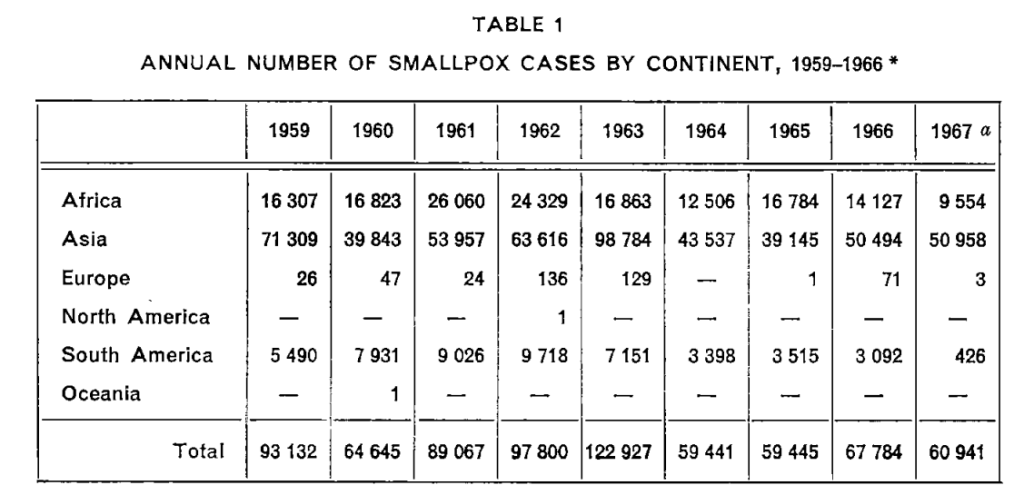
However, 1974 was a particularly bad year with 188,003 cases reported in India alone. A slow decline to zero over the next 3 years does not look at all likely given the incidence data presented here:
When was Monkeypox first reported?
In 1958 a new pox virus was named – Monkeypox. A Danish laboratory had an outbreak of pox in their laboratory monkeys, cynomolgus macaques. Examination under the electron microscope showed it was shaped like a pox virus and the antibodies had similar properties to those produced with Smallpox. Monkeys of the same breed are now used as an animal model for Smallpox. The only thing that distinguished Monkeypox from Smallpox at the time was that Danish researchers could demonstrate disease in mice and rabbits, claiming that “unlike variola it could be maintained in serial intracerebral passages in mice causing encephalitis and in the rabbit skin where it produced severe haemorrhagic lesions.”
There were more reported outbreaks of Monkeypox in captive monkeys in the United States and the Netherlands in the 1960s. No human transmission was seen and researchers concluded that humans were not susceptible.
The first human case of Monkeypox was reported in the Democratic Republic of the Congo. This country had their last official reported Smallpox outbreak in 1968, despite having reported nearly 2,000 cases in 1966. There were 70 reported cases and 18 deaths in the 1968 outbreak. In 1969 there were “several suspected cases… treated… in the hospital but none was confirmed.” However, in 1970 a 9 month old boy presented with two days of fever followed by a pox rash showing a “distribution typical of smallpox”. On day 11 he was admitted to hospital where he was clearly a very sickly child developing other infections and dying of measles after 7 weeks in hospital. There was no reported history of contact with monkeys. There was no disease among the monkey population and no dead monkeys had been identified.
But, since Smallpox had been eradicated two years before, it couldn’t be Smallpox! To resolve this mystery a sample was sent to the WHO Smallpox Reference Centre Laboratory. The people there declared that this was a case of Monkeypox.
How can you tell Smallpox and Monkeypox apart clinically?
The only claimed difference in clinical presentation is that enlarged lymph nodes, which did occur with Smallpox, are allegedly more common with Monkeypox. However, even Edward Jenner described “tumours in the axillae” with Smallpox.
NIAID researchers in USA explained the problem with telling the diseases apart clinically,
“Prior to the eradication of Smallpox, human monkeypox infections were likely misdiagnosed as Smallpox infections due to the prevalence of Smallpox and the similarity of cutaneous disease presentation and progression. Monkeypox was not recognized as a disease distinct from Smallpox until 1970 when the elimination of Smallpox from the Democratic Republic of Congo revealed the continued occurrence of a Smallpox-like disease.”
In 2020, a publication in the WHO bulletin mentioned that, “No concurrent epidemics of Smallpox and monkeypox have ever been reported…With the eradication of Smallpox, monkeypox appears to emerge as the dominant pox disease in humans…We conclude that circulation of Smallpox, followed by worldwide Smallpox vaccination, have previously protected human populations from monkeypox epidemics.”
Smallpox was said to have no animal reservoir
A lack of an animal reservoir was one of the central beliefs upon which the claim of Smallpox eradication could be based. However, questioning during the Monkeypox outbreak revealed that the story was not so simple. There was a report of a monkey having a Smallpox-like rash during the 1968 outbreak and the authors even propose that it might have been Smallpox that was the original source of any issue in monkeys saying: “Contact between monkeys and patients suffering from smallpox is also possible. The local inhabitants informed the investigators that those who are very sick are sometimes isolated in remote areas of the forest. Food is left some distance from the patient and its delivery announced by drum beats. If a smallpox patient died, curious monkeys would investigate the isolation camp and come into physical contact with the corpse.”
Even Donald Henderson, who was credited with leading the eradication of Smallpox, admitted in 1968 that primates could be infected with Smallpox. The WHO report that “a virus, which has been called “whitepox”, that is indistinguishable from variola [Smallpox] virus by laboratory tests has been recovered from the tissues of wild animals.”
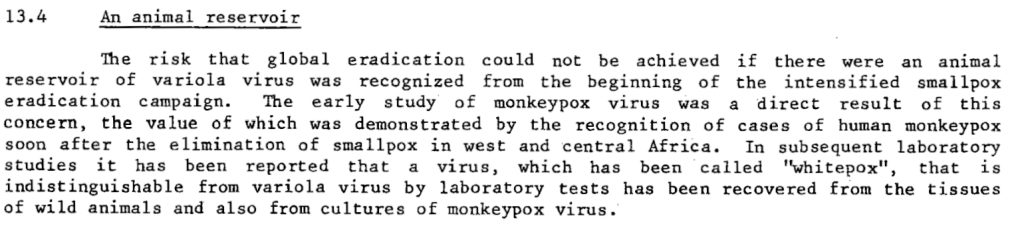
Figure 6: Extract from WHO report commenting on animal reservoirs of Smallpox Page 62
It is now accepted that there is an animal reservoir for Monkeypox, but it occurs in rodents, not monkeys.
What about the rest of the world?
There were 45 cases of Monkeypox diagnosed in Africa in the 1970s.
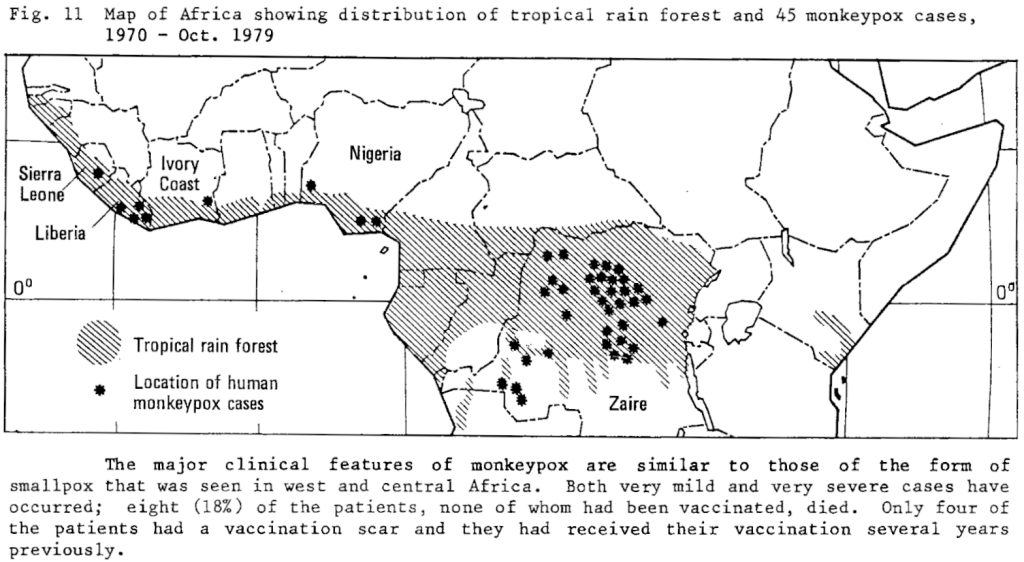
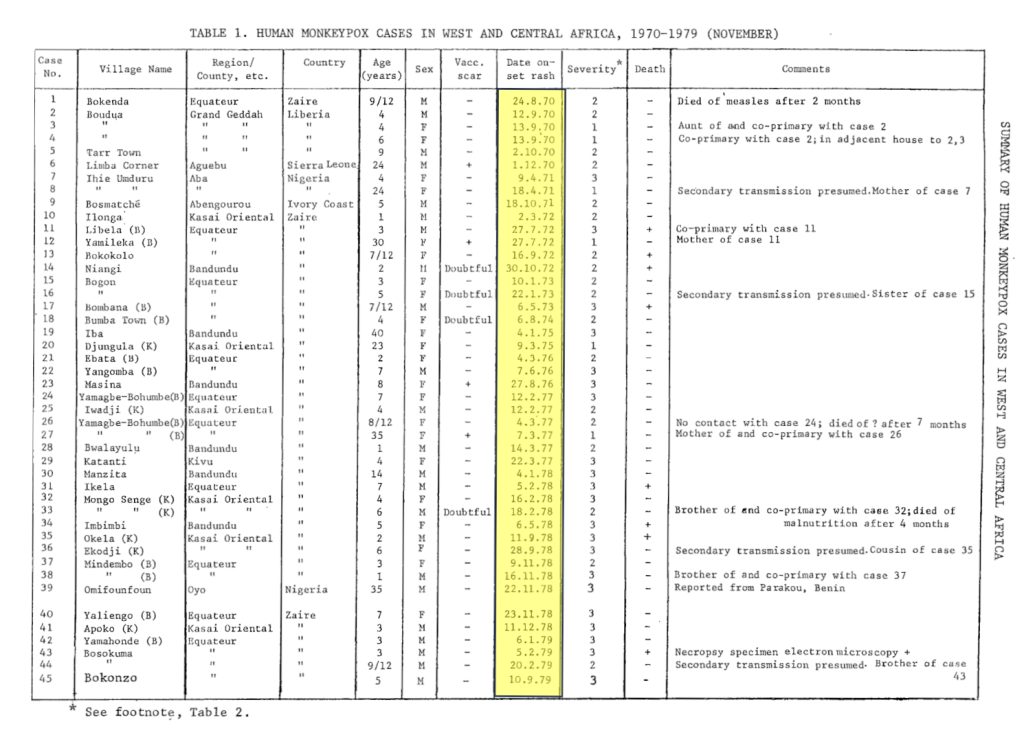
Figure 7: First Monkeypox cases on map above and the dates of diagnosis in a table by WHO
Monkeypox, until recently, was largely confined to Africa. Like Smallpox, it too is an illness which starts with two days of fever before progressing to a similar distribution of pustules. The case fatality rate has been reported to be around 10%, however it is clearly much lower in populations with better underlying health.
India was the other area with a high prevalence of Smallpox in the 1970s. A massive surveillance and vaccination campaign was undertaken. The last case was diagnosed in 1975.
From 1958 Buffalopox was diagnosed in humans in India, “Cases of generalized buffalo pox are often associated with outbreaks of smallpox.” The official story is that Smallpox vaccines given to buffalo evolved into Buffalopox. There are other pox viruses, like Rabbitpox and Horsepox which were said to also have evolved from the vaccine. Full genome analysis, however, showed that they were not vaccine escape variants at all. Buffalopox did not look like the vaccine virus should in egg cultures.
The case fatality rate of Buffalopox (in humans) is 11% and it was first identified as a unique virus in 1977. In 1977 the WHO declared Smallpox eradicated from India. Their own commission reported that year that several municipalities had not reported any fevers or rashes to them of any kind at all! Only a quarter to a third of “chickenpox cases where death had occurred” had samples sent. In several villages a quarter to half of preschool children remained unvaccinated.
More recently, in 2005, 19 cases of a pox outbreak were diagnosed in Pakistan in 5 hospitals, affecting predominantly burns patients along with one member of staff. It was diagnosed as Buffalopox by both the Special Pathogens Unit, National Institute for Communicable Diseases (NICD), Sandringham, South Africa, and the Health Protection Agency (HPA), Centre for Emergency Preparedness and Response, Porton Down, Salisbury, United Kingdom. PCR testing of dressings and ointments did not detect any virus. Further PCR testing of the patient sample for only one gene led to the claim that it was a Buffalopox outbreak. There was no report of any contact with buffalo.
How did the WHO distinguish Monkeypox from Smallpox?
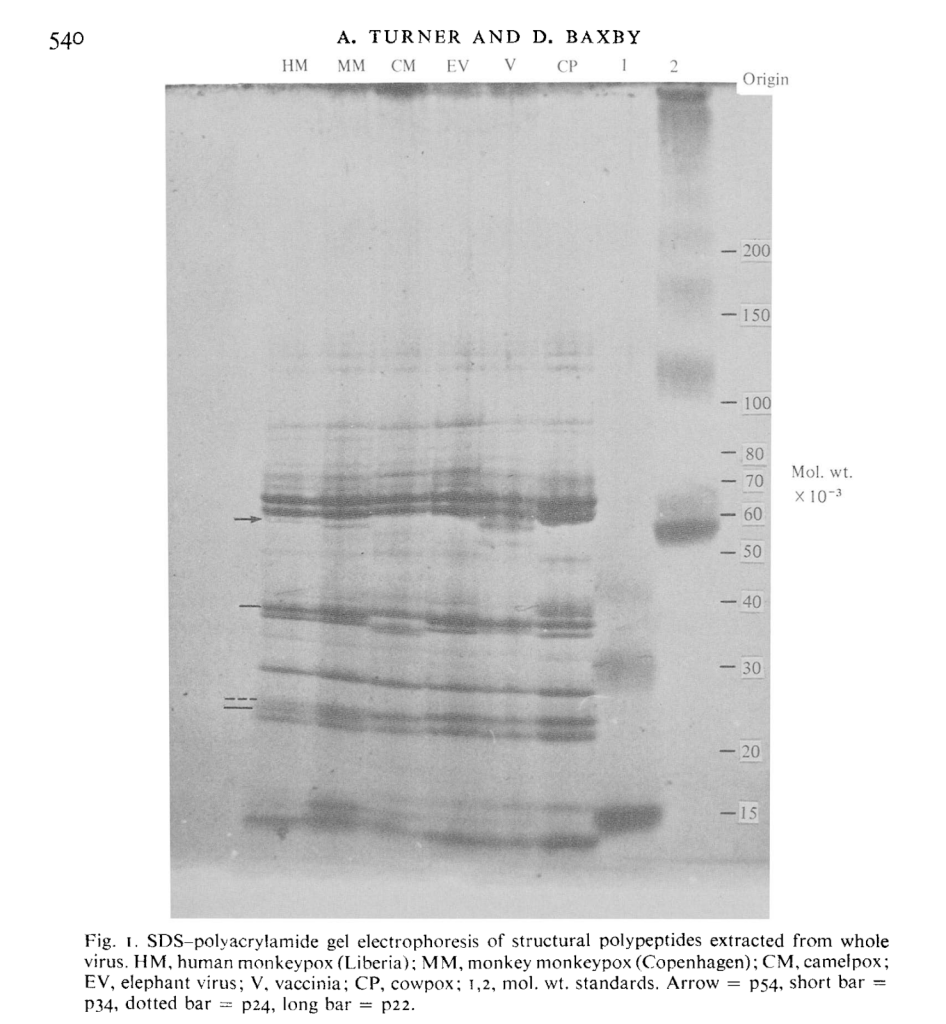
How did the WHO know it was different? It is a critical question. A laboratory technique to enable measuring the size of proteins was first described in 1979 but there was, at that time, no way of sequencing DNA.
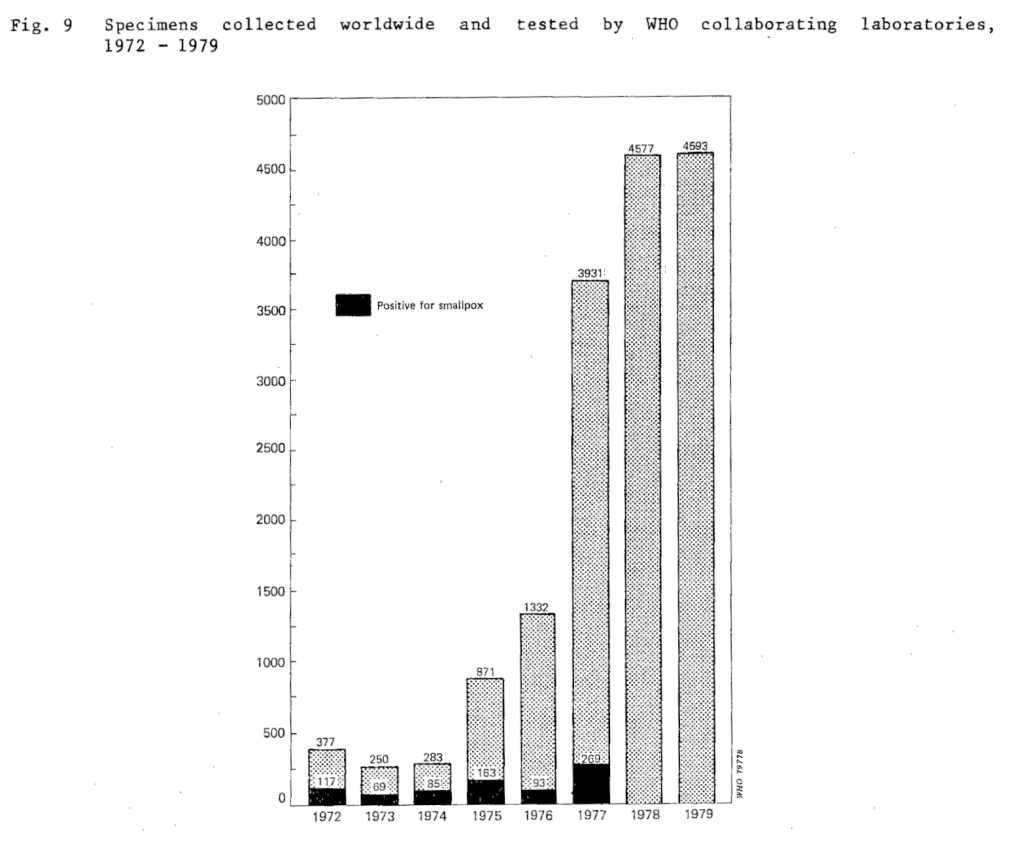
16,000 cases were tested by WHO between 1967 and 1979. They used electron microscopy to distinguish Smallpox from chickenpox but admitted they could not distinguish other pox viruses.
They claimed to be able to distinguish pox viruses by the colour of the lesions made in egg cultures. They were meant to be pink.
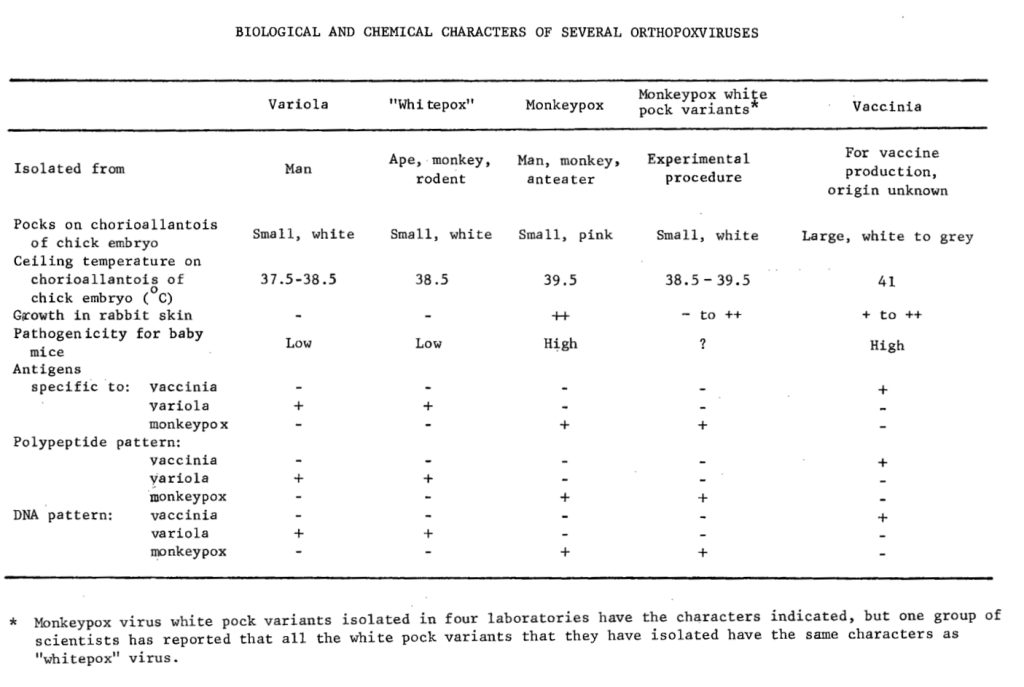
Figure 8 above claims four major differences: the colour of the chick embryo pocks, antigens, polypeptide pattern and the DNA pattern. It was published in 1979, the year that the technique to separate proteins was first published, giving a “polypeptide pattern.”. Others published on the protein differences between pox viruses that year. The method uses a gel and the proteins separate along it in a similar way to chromatography. No significant differences are evident. The sloping of the lines is an artefact of the gel not a real finding.
DNA differences
Fast forwarding to more modern times and there are plenty of claims that DNA sequencing can distinguish these viruses. It is worth remembering, however, that the samples of Smallpox that are being compared have spent decades in a laboratory environment before this testing was possible. One comparison was made with an Indian Smallpox isolate that had spent 25 years adapting to laboratory conditions, one from a Bangladeshi outbreak that had been in the laboratory for nearly 20 years and a Brazilian outbreak from 30 years earlier. Each of these Smallpox viruses had 98% homology to each other in their sequences.
The claim is that small variations, like a deletion in part of a gene called B22R are enough to reliably distinguish Smallpox from Monkeypox. Are these claims consistent enough that anyone could reliably distinguish Smallpox from Monkeypox?
A DNA analysis of a sample from a frozen Lithuanian mummy who died in the 1650s shows that it was fairly different to the Smallpox viruses in the laboratory. Similarly samples from a Czech museum were not that closely related to 20th century variants. In fact they suggested they were closer to ancient versions.
Monkeypox has a sequence of 197,000 letters whereas Smallpox has 187,000. 110,000 of them are almost identical to Smallpox. However, there are deletions and repeats which make up the rest which can result in the claim that overall the sequences are only 96% the same as 20th century Smallpox.
Given the large differences between sequences for different sources of Smallpox, the claim that Monkeypox is a very different virus (especially as it is indistinguishable clinically) starts to look weak.
Were huge vaccination campaigns really the reason these outbreaks stopped?
Globally, the triumph of the official eradication of Smallpox led to the assumption that the mass vaccination campaigns could be wound down.
The WHO goes into great detail about how vaccination must be performed in the upper layers of the skin – the epidermis. Deeper vaccination “has relatively little immunising capacity.” They also report how the intervention that actually broke transmission chains was surveillance and stopping contacts. “Eradication campaigns based entirely or primarily on mass vaccination succeeded in some countries but failed in most. Mass vaccination campaigns were most successful in countries with relatively well developed and well managed health services, adequate reporting systems, and reasonably good communications…However, in some countries, even when vaccination coverage reached 80% or even 90% the remaining susceptibles, grouped in particular parts of the country or in lower socioeconomic areas of cities, provided a sufficiently large population for smallpox transmission to continue…In heavily populated portions of Java, where the vaccination coverage had reached levels of over 90%, transmission continued until active surveillance detected outbreaks and they were contained.”
The first report of Monkeypox revealed the WHO’s utter confidence that Smallpox vaccination would protect against Monkeypox, “because of the very high level of vaccination immunity in this population, it is entirely possible that the patient was not in effective contact with susceptible persons.” Similar references to Smallpox vaccination protecting against Monkeypox is evidenced throughout the WHO reports and more recently, when the WHO claimed a Monkeypox emergency, the gay population were given Smallpox vaccines. The fact gay men, who have a higher rate of HIV related immune suppression, were more susceptible, again suggests host factors are key to susceptibility.
Some may find it paradoxical for the WHO to simultaneously admit to the vaccination providing less than perfect immunity against Smallpox whilst claiming complete confidence in its effectiveness against Monkeypox and Buffalopox. They may also be curious about the fact that those diseases emerged at the time Smallpox was being eradicated through mass vaccination, never having been thought to have caused disease in humans before.
Perhaps we are overcalling the issue here. Perhaps genomics really is accurate enough to distinguish these different pox viruses reliably despite hugely variable laboratory conditions.
It is worth pointing out that even if they are genetically distinct, the question must arise as to whether the viral ecological niche is the same, but has been filled by a cousin. In practical terms, the difference for human health appears to hold limited significance, if any.
However, the role that the Smallpox eradication narrative plays in science and medicine is so vast that the implications of questioning its foundations cannot be overstated.
