
Only 14 pregnant women currently on ICU
When deaths and cases are not frightening enough the media turn, as they did last year, to pregnant women to promote fear. Media claims that 1 in 5 women in critical care are pregnant are false. There were 20 pregnant women out of 118 total patients since July who have been on “ECMO”, a lung support machine which oxygenates the blood outside the body. No-one in the whole country was put on ECMO for COVID in the last week reported (figure 1). Prioritising pregnant women for such therapy would be a reasonable approach so the proportion receiving this care would not necessarily reflect the proportion of pregnant women who were sick on intensive care.
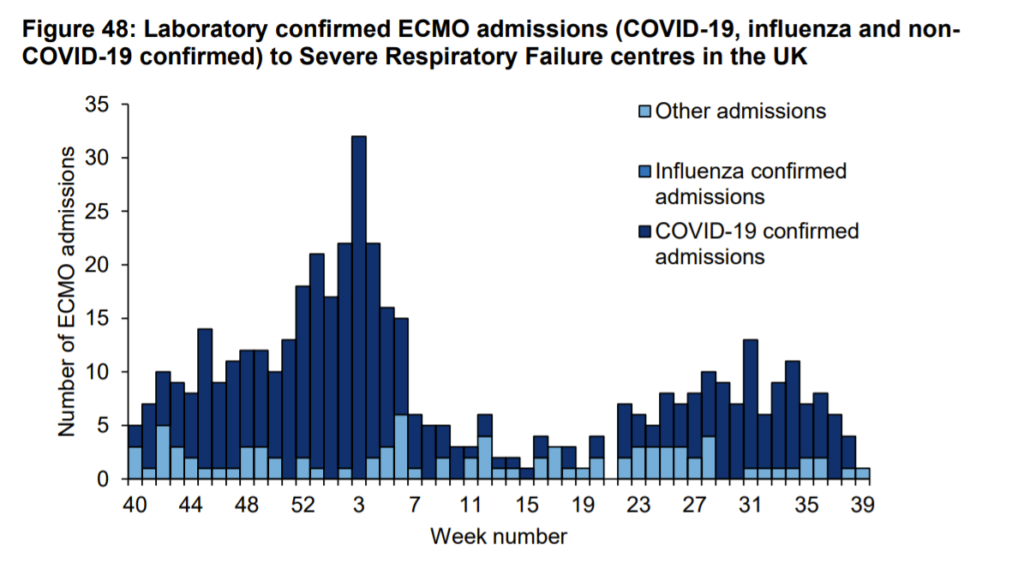
Figure 1: Use of lung support machines (ECMO – extra-corporeal membrane oxygenation)
However, as of 8th October, there were only 14 pregnant women in intensive care (ICU) out of a total of 890 male and female patients, i.e. pregnant women accounted for 1.6% of all patients in ICU. There are at least 480,000 women who are currently pregnant.
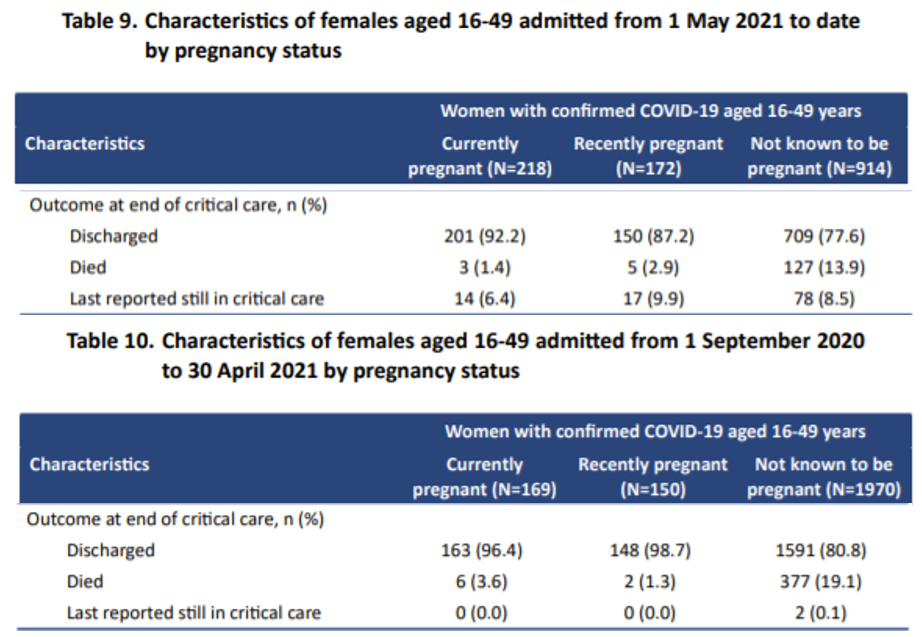
Figure 2: Latest data on ICU patients compared to second wave
The mortality rate among pregnant women is one tenth that of non-pregnant women aged 16-50 years (figure 2). The decline in mortality has been greater in pregnant women since vaccination than in non-pregnant women. COVID ICU mortality rate is twice as high as the background ICU mortality rate for non-pregnant women but only slightly higher for pregnant women. Since September 2020 six pregnant women on ICU have died and 16 pregnant or recently pregnant women. To put that number into perspective it is worth comparing the pre-COVID total risk of dying with that for pregnant and non-pregnant women since September 2020 with a COVID positive test (figure 3).
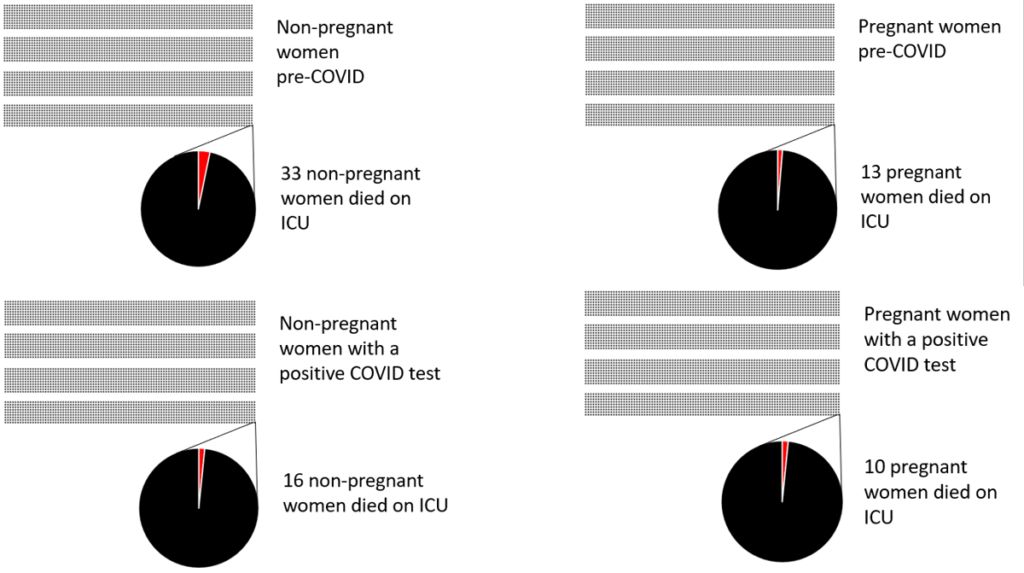
Figure 3: Total deaths per 400,000 women from pregnant and non-pregnant (aged 16-50) populations annually pre-COVID and since September 2020 with a COVID positive test result. Each dot represents 100 women and the final dot is expanded to show the deaths in that population.
Over the course of the whole pandemic there have been 416 pregnant women admitted to ICU with a COVID label out of 43,922 total admissions (<1%). In a normal year pregnant women account for 0.8% of ICU admissions.
Pregnancy comes with risk. Thankfully the risks are small but they have not been eliminated. Prior to COVID, about 300 pregnant women a year were admitted to ICU, in the context of around 640,000 births a year this translates to around1 in 2000. A further 1,400 women who had recently been pregnant were also admitted per year. Together these made up 14% of intensive care admissions for all women aged 16-50 years of age. The admission rate since COVID has increased and 1 in 1,500 pregnant women have been admitted to ICU with a positive COVID test result. In the same period 1 in 4,000 non-pregnant women of child bearing age were admitted to ICU with a COVID diagnosis.
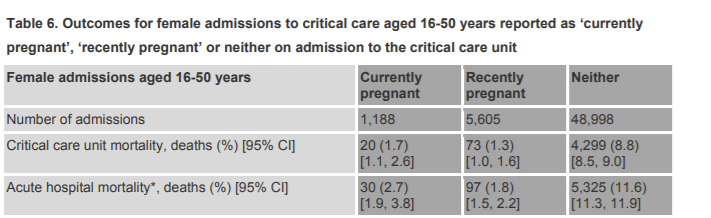
Figure 4: Pre-COVID ICU admissions of pregnant and non-pregnant women
| Pregnant or recently pregnant (% of admissions) | Non-Pregnant women aged 16-50 (% of admissions) | |
| Pre-COVID per year | 23 (1.7%) | 1075 (8.8%) |
| COVID (since Sept 2020) | 16 (2.3%) | 504 (17.4%) |
| Non-COVID (since Sept 2020) | ? | ? |
Table 1: Annual ICU mortality per ICU admission pre and post COVID
COVID does appear to cause higher numbers of people to need intensive care compared to even a bad influenza variant. However, the numbers involved remain small. Respiratory failure has always been the most common cause for a pregnant woman to need admission to ICU and more than 1 in 5 pregnant women on ICU were there for pneumonia. In the past many of these pneumonias will have been due to influenza but more recently they have been caused by COVID.
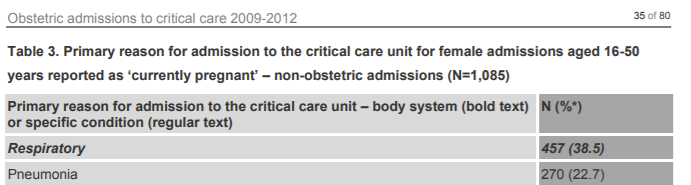
Figure 5: Pre-COVID reasons for admission of pregnant women to ICU
Of those pregnant women in hospital last year, 1 in 3 of those testing positive had no symptoms at all. The numbers of positive PCR results are disproportionately high for women of child bearing age who are much more likely to be tested routinely as part of their antenatal care and are therefore at higher risk of meaningless positive test results.
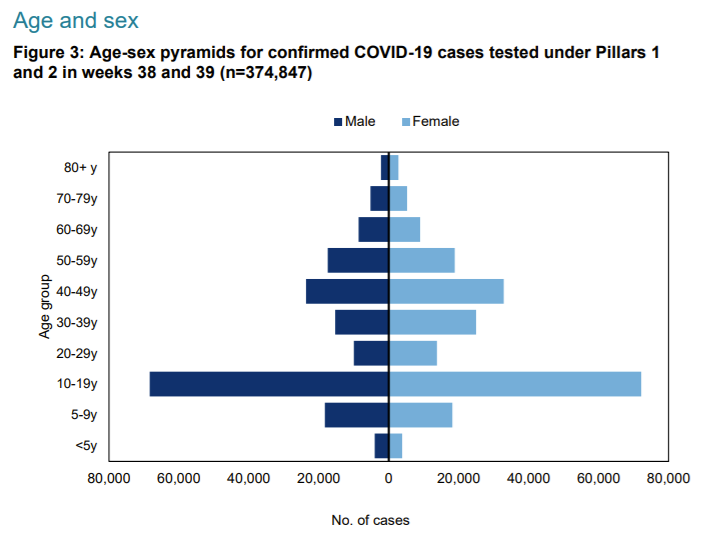
Figure 6: Positive test results by age and sex from PHE
Overall deaths in women of child bearing age rose in Spring 2020 and Winter but have been at expected levels since. Mortality of women on ICU has fallen from 19% in winter to 14% in those who are not pregnant and 2.6% to 2.3% in those who are pregnant or have been recently (see figure 2).
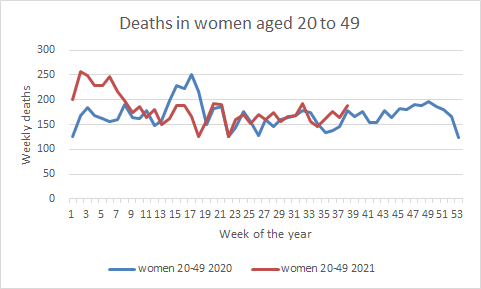
Figure 7: Total mortality by week for women of child bearing age
Conclusion
Pregnancy has always come with low risk of complications. The risk from COVID is slightly higher than the risk presented prior to COVID but is of a similar order of magnitude. The risk of dying on ICU with a COVID diagnosis was ten times higher in the non-pregnant population of women of child bearing age. The mortality rate has halved for pregnant women whereas the fall among the non-pregnant population, more of whom are likely to have been vaccinated, has been only 27%. The risk of being admitted to ICU with a COVID diagnosis was higher in pregnant women than non-pregnant women. Although this appears contradictory, they may be prioritised for admission and there will be pregnant women included who were in ICU for other reasons and had incidental meaningless positive test results which may have inflated these figures.

