
Two views of the Midazolam story
It is important that we admit what we do not know and there are many gaps to the end of life Midazolam story. In fact it is possible to interpret what we do know in two totally different ways.
- The relatives have been deceived
- The relatives are right
Here are a number of people who honestly believe that their relatives were not necessarily bound to die from covid, but died prematurely as a direct result of being treated with midazolam.
Are they right?
1. The relatives have been deceived
The first argument is that a lack of contact and breakdown in communication between relatives and medical staff meant that these relatives did not appreciate how close to death their loved ones were. The healthcare staff were certain that they had no hope of turning a corner. The healthcare staff were correct about this. They therefore initiated care that would ease distress. Midazolam reduces respiratory drive and that means a much more peaceful passing for those struggling to breathe. Midazolam and morphine are effective treatments that do not reduce the time to death in a palliative care setting. Unfortunately, the breakdown in communication continued afterwards and was confounded by online campaigners claiming many people had died because of midazolam.
2. The relatives are right
The alternative argument is that midazolam and morphine did accelerate death in these patients with an acute respiratory tract infection. They are both known to reduce the respiratory drive yet there were centralised protocols which included these drugs for covid patients and staff were told that they “should not be withheld because of an inappropriate fear of causing respiratory depression.” That guideline was meant for community care but a similar message was also present in training documents from Health Education England for hospital care, telling doctors “don’t be afraid to prescribe in line with your patient’s requirements.”
Figure 1 below shows guidance recommending midazolam and morphine to treat breathlessness and goes on to say:
“Patients with severe COVID-19 symptoms, especially severe breathlessness, who are not expected to survive their illness often deteriorate quickly over a short period of time. As a result, they may need a higher starting and maintenance doses of opioids / anxiolytics than suggested previously for breathlessness and associated anxiety.”
Let’s dissect this carefully.
Firstly, doctors are being taught that they cannot rely on their clinical acumen to determine when someone is near death because they “often deteriorate quickly.” Then the question becomes who is “not expected to survive their illness”? How were doctors to judge that? The general public based their assessment of the risk from covid on the government’s response to it. Those in charge were reacting as though it was really life-threatening, so it must be true. Is it possible doctors were doing the same? Worst of all, were deaths due to midazolam and morphine actually giving these doctors the impression that the risk of death was much higher than it actually was, when in fact it was the protocol that ended their life, not the disease? Did this create a lethal feedback loop where premature deaths were assumed to have been ‘inevitable’, due to an incorrect risk-assessment and then were also assumed to have been caused, not by intervention, but by covid?
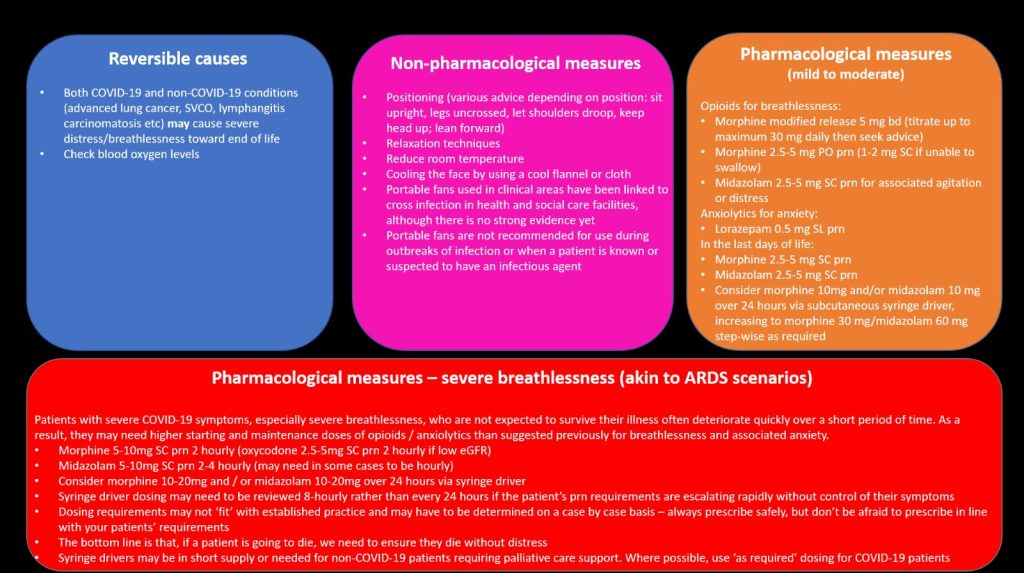
Figure 1: Health Education England summary of interventions to be used in covid including using Midazolam and morphine to treat breathlessness.
These included pathways where anyone who was not fit for ventilation was directed towards a possible palliative approach:
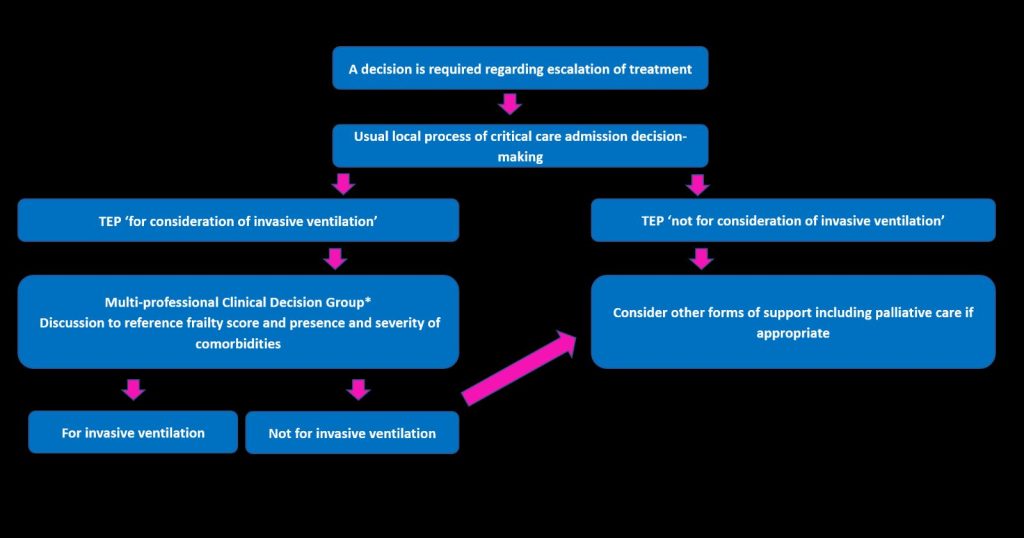
Figure 2: Health Education England treatment pathway
A training video shows a doctor prioritising comfort over treatment (4:30):
“If you become more unwell, we would do everything we could to make sure we get you comfortable. Also… we would do everything we could actively as we’re doing now to try and treat you and get you better.”
The evidence that these drugs do not reduce the time to death is based on patients dying mostly of cancer and heart failure rather than an acute respiratory infection where the respiratory drive may be life saving. Struggling to breathe can indeed be distressing and is also distressing for those around, including healthcare staff. Staff who can provide a medication that alleviates this struggling may well feel they are practising the very best of medicine, but if they are also removing a life saving drive to breathe they may in fact be accelerating or even precipitating death.
If scenario 1 is right then the best thing to do would be to have a full investigation. The details of these cases need to be fully understood by the relatives and any concerns could be laid to rest by a thorough, open exploration and explanation of what actually happened.
If scenario 2 is right then there needs to be a full investigation so we can learn about when these drugs might in fact be dangerous and ensure no further lives are lost.
The solution is the same regardless of the underlying problem here. Proper investigation is needed. HART have been calling for such an investigation since June 2021, yet there is still no sign of it happening, to the growing frustration of grieving relatives.
